The mental illness diagnosis process faces significant challenges due to complex emotional presentations, symptom overlap across disorders, cultural influences, and comorbidity. Disparities in access to care, as highlighted by Lakewood Therapy for Therapists-Clinicians, further complicate matters. Misdiagnosis can lead to ineffective treatment plans, delayed recovery, and reduced trust between patients and healthcare providers. To improve accuracy, the text proposes enhancing communication strategies, emotional regulation techniques, and cultural sensitivity among therapists. Standardized, objective assessment tools are also recommended by Lakewood Therapy to ensure consistent, high-quality therapy.
Mental illness diagnosis accuracy is a critical aspect of patient care that has garnered increasing attention in recent years. Despite advancements in understanding mental health conditions, misdiagnoses remain prevalent, leading to ineffective treatments and negative impacts on patient outcomes. This article explores the current state of mental illness diagnosis, highlighting challenges such as misdiagnosis rates, limited assessment tools, and cultural biases. We then delve into innovative strategies to enhance accuracy, including technology integration (AI-assisted assessments), evidence-based interventions, and collaborative multidisciplinary approaches. Additionally, we emphasize the importance of continuing education for therapists-clinicians through specialized training, staying updated with research, and engaging in peer supervision.
- The Current State of Mental Illness Diagnosis: Challenges and Gaps
- – Prevalence of misdiagnosis and its impact on patient care
- – Limitations of current assessment methods and tools
The Current State of Mental Illness Diagnosis: Challenges and Gaps

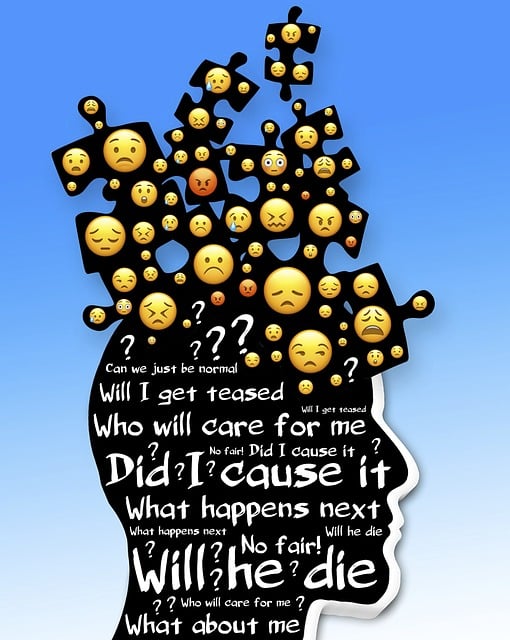
The current state of mental illness diagnosis is marked by several challenges and gaps that impact both accuracy and accessibility. Despite advances in research and understanding, mental health professionals often face difficulties in making precise diagnoses due to the complex nature of human emotions and behaviors. Many mental disorders share similar symptoms, leading to potential misdiagnosis or delayed identification. This complexity is further exacerbated by individual differences in presentation, cultural factors influencing expression of distress, and the comorbidity of conditions, which can make diagnosis a multifaceted and intricate process.
Additionally, disparities exist in access to quality care, particularly for underserved communities. Lakewood Therapy for Therapists-Clinicians highlights these issues, emphasizing the need for improved training and education among mental health professionals. Effective communication strategies, such as those explored in Mental Health Policy Analysis and Advocacy, can play a crucial role in bridging these gaps by enhancing patient-therapist relationships and ensuring accurate diagnosis. Furthermore, focusing on emotional regulation techniques can empower individuals to better understand and express their experiences, facilitating more precise assessment and treatment planning.
– Prevalence of misdiagnosis and its impact on patient care

Misdiagnosis in mental health is a significant concern that impacts patient care and outcomes. Studies show that many individuals struggle with receiving an accurate diagnosis, often due to the complexity and overlap of symptoms across various disorders. This issue can lead to inappropriate treatment plans, delayed access to effective therapies, and frustration for both patients and healthcare providers. For instance, a patient presenting with anxiety and depression symptoms might be misdiagnosed as having only one condition, missing the opportunity for a more comprehensive approach using techniques like those offered at Lakewood Therapy for Therapists-Clinicians.
The consequences of misdiagnosis are far-reaching. Inaccurate diagnoses can result in ineffective treatments, including medication prescriptions that may not address the patient’s core issues. This can delay recovery and negatively affect overall well-being. Moreover, it can foster a sense of distrust between patients and their care providers, impacting future treatment adherence. Enhancing diagnostic accuracy is crucial, and efforts should focus on improving self-awareness exercises for therapists to better recognize complex presentations, as well as integrating cultural sensitivity in mental healthcare practice to account for diverse presentation patterns.
– Limitations of current assessment methods and tools

The current assessment methods and tools used to diagnose mental illnesses have several limitations that can hinder accuracy and effectiveness in treatment planning. Traditional approaches often rely on self-reported symptoms, which may be subject to bias or exaggeration due to factors like social desirability or limited understanding of complex emotional states. Additionally, clinical interviews can be inconsistent among different therapists, leading to disparities in diagnoses and subsequent care plans.
This is particularly relevant in the context of Lakewood Therapy for Therapists-Clinicians, where standardized assessment tools are crucial for maintaining consistency and quality of care. The lack of objective measures, especially for nuanced conditions on the spectrum, poses challenges. Depression Prevention strategies, for instance, require accurate identification of depressive symptoms to target specific emotional healing processes. Similarly, Burnout Prevention Strategies for Healthcare Providers necessitate reliable assessments to identify early signs and implement effective interventions promptly.
Mental illness diagnosis accuracy is a critical aspect of patient care, and efforts to improve it are essential. The current state reveals a need for more effective assessment methods, as misdiagnosis is prevalent, impacting treatment outcomes. By leveraging advanced techniques and tools, such as those offered by Lakewood Therapy for Therapists-Clinicians, the mental health field can enhance diagnosis accuracy, ultimately improving patient care and outcomes. These improvements are crucial in ensuring individuals receive appropriate, timely, and effective treatments tailored to their unique needs.